Drug development: No Mom Left Behind
 |
| Photo by Kendal on Unsplash |
Historically, during drug and vaccine development, pregnant women were rarely included in clinical trials due to ethical considerations
and, more importantly, concerns over safety in pregnancy and fetal health. During the recent Ebola outbreak,
pregnant women were denied access to Ebola vaccines—although this decision was reversed months later in February 2019. While the safety and ethical concerns for pregnant
mothers and their fetuses regarding experimental drugs definitely have their
merits, this raises the question on how we can improve the drug development
pipeline to equally benefit everyone later on. No one should be left behind.
As the world is rushing to develop drugs and vaccines
for the new rapidly-spreading life-threatening coronavirus disease (COVID-19), we may need to revisit the topic of how we can make sure that everyone, including pregnant women,
will equally benefit from the life-saving drugs and vaccines amidst a pending
pandemic. Unlike previously known viruses, such as Zika, at the moment,
there is no evidence to show that COVID-19 can pass from pregnant mothers to
their babies. Although this study is limited to mothers exposed to COVID-19 viruses
at later stages of pregnancy. Nevertheless, this brings up a good point on how
we can include some of the most vulnerable populations (pregnant mothers) in drug or vaccine development pipeline.
There is a long road ahead for researchers, clinicians and
the public to find a middle ground on the inclusion of pregnant mothers during
a clinical trial for a new drug or vaccine. The threats on fetal health, whether from the diseases themselves or potential adverse effects of the drugs, make it nearly impossible to design and implement appropriate protocols. The good news is that there is a bioengineering technology that can help bypass these issues regarding drug testing for pregnant women by the use of tissue models that can mimic the biology of the uterus in the lab.
The use of uterine organoids (mini-organ in a dish) allows scientists to study the physiology of the uterus as well as disease modeling and drug testing in the lab. This tissue engineering technique can be used further to mimic pregnancy condition. This platform has the potential to help researchers assess the effects and safety of experimental therapeutics in pregnant women.
Here in our lab, we are using uterine organoids generated from the endometrium (the lining of the uterus) to
understand how certain viruses, in our case, Zika virus, can infect the uterus, and transmit from pregnant
mother to her fetus. We are developing ways to prevent this transmission by testing candidate anti-Zika antibodies on these organoids. These organoids made for the drawbacks of traditional cell culture as they retain similar physiology to the real organ, and they bypass direct human testing. Disease modeling and drug testing on this system, therefore, are more applicable in clinical settings. This uterine mini-organ can be a powerful platform to test for effects and safety of candidate therapeutics regarding pregnant women as a part of drug and vaccine development. We hope that our study can help improve healthcare quality to ensure well-being for pregnant women and their newborns.
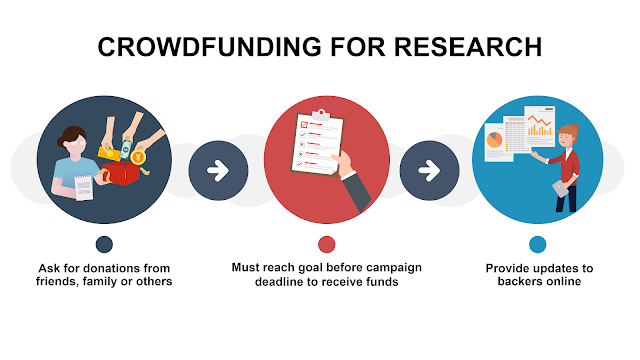
We are launching a crowdfunding campaign soon on a project titled "Blocking Zika Mother-to-Child Transmission". Stay tune.
We are launching a crowdfunding campaign soon on a project titled "Blocking Zika Mother-to-Child Transmission". Stay tune.


Comments
Post a Comment